Unexplained Bruises? When to Be Concerned and What Could Be Causing Them
Bruises are common occurrences in everyday life—minor injuries, knocks, or bumps often result in discoloration of the skin as blood collects under the surface. Most bruises are harmless and fade over time, but sometimes bruises appear spontaneously or without a clear explanation, raising concerns about underlying health issues. In this comprehensive article, we will explore what unexplained bruises might indicate, when you should seek medical attention, possible underlying causes, diagnostic approaches, and available treatments and management strategies. We will also discuss special populations, lifestyle factors, and prevention tips.
What is a Bruise and How Does It Form?
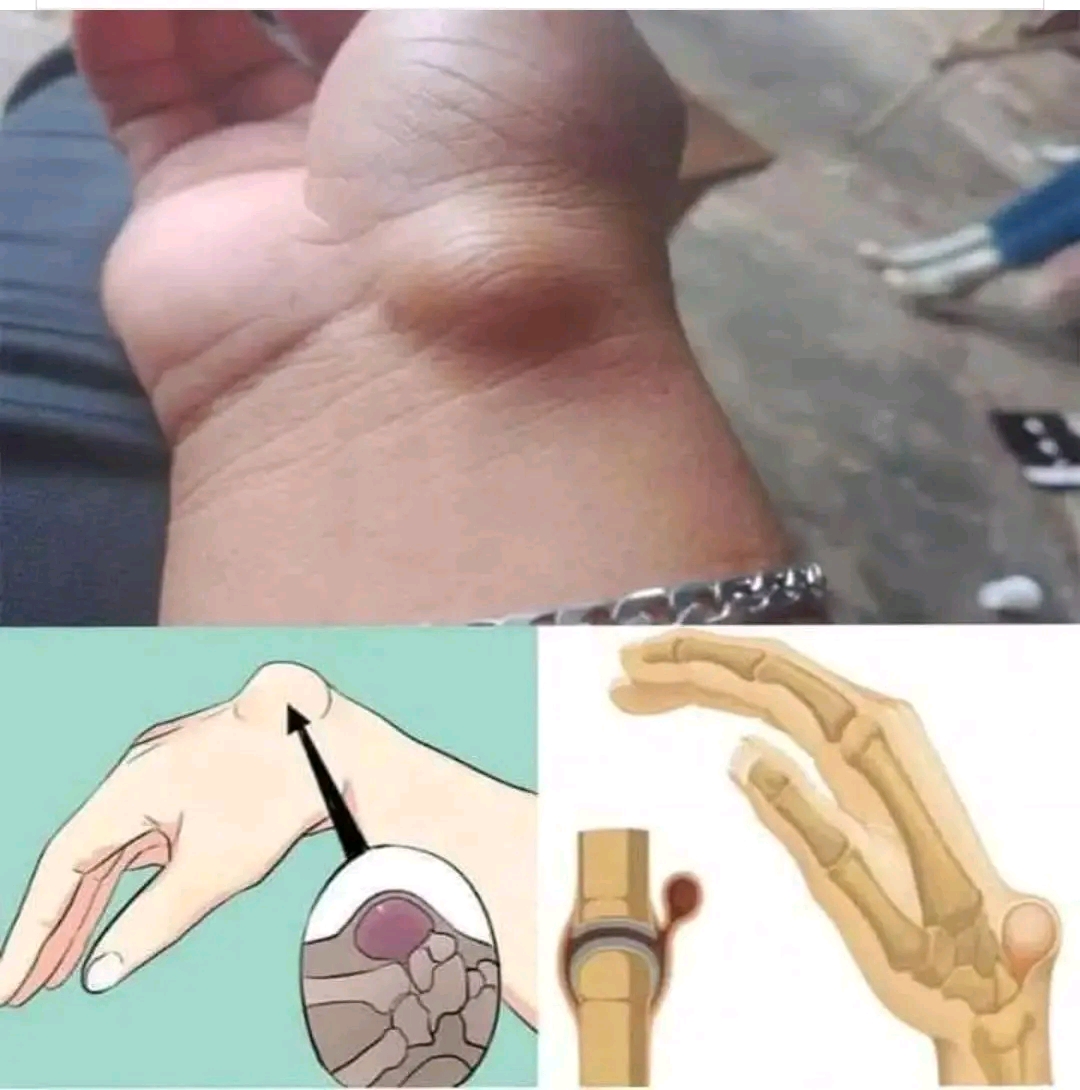
A bruise, medically referred to as a contusion, forms when small blood vessels (capillaries) beneath the skin rupture, often due to trauma. Blood leaks into surrounding tissues, causing discoloration—initially red or purple, later turning blue, green, yellow, and finally brown as the body breaks down the blood cells. The stages of color change typically correspond to the bruise’s age. While minor injuries are the most common cause, unexplained bruises may arise from a variety of other medical, nutritional, or systemic factors.
When Is an Unexplained Bruise a Cause for Concern?
Occasional, isolated bruises are rarely a cause for alarm. However, you should consider seeking medical attention if you notice any of the following:
multiple bruises appearing without injury persistent or unusually large bruises bruises that take an unusually long time to heal bruising in unusual locations, such as face or trunk recurrent bruises accompanied by other symptoms like fatigue, nosebleeds, bleeding gums, or joint pain bruising associated with swelling or severe pain unexplained bruising in a child or infant unexplained bruises in the elderly or frail individuals taking blood‑thinning medication (“blood thinners”) unexplained bruising along with weight loss, fever, or night sweats unexplained bruising that appears after starting new medications or supplements bruising coupled with a family history of bleeding or clotting disorders
If any of these scenarios apply, it is important to consult a healthcare provider for evaluation.
Possible Underlying Causes of Unexplained Bruises
- Minor Trauma or Accidental Bumps
Even when you don’t recall hitting or bumping into something, minor unremembered trauma can cause bruises. Elderly people, those with poor vision, or individuals with decreased mobility may be more prone to unnoticed injuries. Thinner skin, which commonly occurs as we age, leads to capillaries being more fragile and vulnerable to rupture. - Medications and Supplements
Certain medications increase susceptibility to bruising. These include anticoagulants (e.g., warfarin, heparin), antiplatelet agents (e.g., aspirin, clopidogrel), corticosteroids (e.g., prednisone), selective serotonin reuptake inhibitors (SSRIs), nonsteroidal anti‑inflammatory drugs (NSAIDs), and topical or systemic steroids. Herbal supplements—such as ginkgo biloba, garlic, fish oil, vitamin E, and high‑dose niacin—may also impair clotting mechanisms or thin the blood. - Platelet Disorders
Platelet count or function abnormalities may lead to easy bruising. Thrombocytopenia (low platelet count) can stem from conditions like immune thrombocytopenic purpura (ITP), bone marrow suppression (e.g., leukemia, aplastic anemia), or medication‑induced causes. Even when platelet count is normal, platelet function disorders (e.g., von Willebrand disease, acquired platelet dysfunction) can cause bleeding and bruising. - Coagulation Factor Deficiencies
Disorders such as hemophilia A or B, or von Willebrand disease, involve deficiencies in clotting factors, leading to prolonged bleeding. While usually diagnosed early in life, mild forms may go unnoticed until later. Liver disease can impair production of clotting factors, likewise vitamin K deficiency may hinder the clotting cascade. - Connective Tissue Disorders
Disorders affecting collagen or vascular integrity—such as Ehlers‑Danlos syndrome or scurvy (vitamin C deficiency)—can result in fragile blood vessels. In scurvy especially, bruising often appears in areas under stress or pressure (e.g., legs, shins) and may be accompanied by gum bleeding, corkscrew hairs, or perifollicular hemorrhages. - Systemic Diseases
Underlying illnesses may manifest with bruising: • Liver disease (e.g., cirrhosis) — reduced synthesis of clotting factors
• Kidney disease — platelet dysfunction or toxin-induced coagulopathy
• Blood cancers — leukemia may cause thrombocytopenia or abnormal vessel integrity
• Infection — sepsis can impair clotting mechanisms or cause disseminated intravascular coagulation (DIC)
• Autoimmune diseases — such as systemic lupus erythematosus (SLE) with secondary effects on blood and vessels - Vascular Conditions
Vasculitis—inflammation of blood vessels—can lead to purpura or ecchymoses. Conditions like Henoch‑Schönlein purpura (IgA vasculitis) may especially affect children, with bruising, abdominal pain, or kidney involvement. In older individuals, senile purpura (dermatoporosis) results from sun‑damaged, fragile skin that bruises easily. - Malnutrition and Nutrient Deficiency
Certain deficiencies, such as vitamin C (scurvy), vitamin K, vitamin B12, and folate, can impair blood vessel integrity or clotting factor production. Older adults or those with malabsorption, alcohol misuse, or restrictive diets may be at higher risk. - Cancer and Malignancy
Leukemia, lymphoma, or multiple myeloma may affect bone marrow production of platelets or clotting factors. Solid tumors can also cause coagulopathy or paraneoplastic syndromes leading to increased bruising. - Rare Causes
Rarely, unexplained bruising may be linked to inherited bleeding disorders like Glanzmann thrombasthenia, rare coagulopathies, or factitious disorder (self‑inflicted bruising). Psychological factors, such as stress or emotional abuse, may also play roles in some cases.
Special Populations: Children, Elderly, and Pregnant Individuals
Children
Unexplained bruises in children, particularly infants who are not mobile, are a red flag and merit immediate evaluation for potential abuse or underlying medical disorders. Bruising over the ears, neck, trunk, or patterns like hand‑prints or belt‑marks should prompt urgent investigation. Pediatric conditions like ITP, leukemia, or vascular malformations should be ruled out.
Elderly
Thinning skin and fragile capillaries, often worsened by sun damage and corticosteroids, cause easy bruising. Aging skin also heals more slowly. Fall risk and poor vision compounds bruising risks. However, unexplained or large bruises still warrant evaluation, especially to rule out bleeding disorders or medication side effects.
Pregnancy
Pregnancy induces many changes: increased blood volume, altered platelet function, and potential for gestational thrombocytopenia. Additionally, increased falls or accidents due to changes in balance may cause bruises. However, unexplained bruising should prompt evaluation for preeclampsia‑related coagulopathy or undiagnosed bleeding disorders.
Signs That Warrant Immediate Medical Attention
If bruising is accompanied by any of the following, seek emergency care: significant bleeding that doesn’t stop after 10–15 minutes deep muscle or joint pain and swelling infected-appearing or rapidly spreading bruise signs of anemia (pallor, rapid heart rate, fainting) …or systemic symptoms such as fever, fatigue, night sweats, weight loss If there is a history of abuse or you suspect foul play, it is ethically and legally important to involve appropriate protective services.
How Doctors Evaluate Unexplained Bruises
History
A detailed history includes onset, frequency, size, and location of bruises; any associated symptoms (bleeding gums, nosebleeds, joint pain); medication use (including supplements/herbals); personal or family history of bleeding disorders; alcohol use and liver disease; nutritional status and dietary habits; history of injuries or falls; in children, careful social context evaluation; in elderly, fall risk and home environment.
Physical Examination
The physician evaluates bruises—size, shape, color, distribution, and pattern—and looks for signs of petechiae (tiny pinpoint hemorrhages), purpura (larger non‑blanching spots), or systemic signs such as enlarged spleen or lymph nodes. Skin integrity, signs of sun damage, signs of trauma, or needle marks (in cases of intravenous drug use) are also assessed.
Laboratory Investigations
– Complete blood count (CBC) with platelet count (thrombocytopenia or anemia)
– Peripheral blood smear (platelet morphology, blasts, schistocytes)
– Coagulation panel: prothrombin time (PT), activated partial thromboplastin time (aPTT), international normalized ratio (INR)
– Liver function tests and kidney function tests
– Vitamin levels (vitamin C, K, B12, folate)
– Specific tests: von Willebrand factor antigen/activity, factor VIII/IX assays, platelet function tests
– Additional tests as indicated: autoimmune markers (ANA, anti‑dsDNA), viral hepatitis panels, HIV test, D‑dimer, fibrinogen.
Imaging and Further Diagnostics
In more complex cases, imaging may help: ultrasound of the abdomen for organomegaly, CT or MRI to locate internal bleeding, bone marrow biopsy for suspected leukemia, and skin biopsy if vasculitis is suspected.
Treatment and Management
Address Underlying Cause
Treat any identified deficiency (vitamin C or K supplementation), manage liver disease, adjust medications if needed (e.g., altering dosage of anticoagulants), and treat autoimmune or hematologic disease appropriately.
Supportive Care
Apply cold compresses early after bruising to reduce bleeding and swelling, followed by warm compresses after 48 hours to increase circulation and healing. Elevation of the affected area helps reduce swelling. Protect areas prone to injury.
Topical Treatments
Over‑the‑counter topical arnica gels, vitamin K creams, or heparinoid creams may help speed bruise resolution, though evidence varies. Gentle massage (only after the bruise has matured past the red/blue phase) may improve circulation.
Pain Management
If bruises are painful, acetaminophen (paracetamol) is preferred over NSAIDs, which may worsen bleeding. Always discuss pain relief options with your healthcare provider.
Lifestyle and Dietary Measures
Maintain a balanced diet rich in fruits, vegetables, and sources of vitamin C (e.g., citrus fruits, berries, broccoli), vitamin K (leafy greens), and protein for tissue repair. Stay hydrated. If you smoke, consider quitting, as smoking impairs blood vessel integrity. Engage in gentle strength and balance exercises to reduce fall risk, especially in elderly individuals.
Follow‑Up and Monitoring
Track bruise frequency, size, healing times, and any new symptoms. Follow up with your healthcare provider to adjust treatment, repeat lab tests, or refer to specialists (hematologists, dermatologists, rheumatologists) if needed.
Prevention Tips
Protective Clothing
Wear long sleeves or padded garments during activities where minor bumps are likely, especially for individuals with fragile skin or clotting issues.
Modify Your Environment
Improve indoor lighting, remove tripping hazards, use non‑slip mats, and install handrails to reduce falls. In the elderly, ensure footwear supports balance and strength.
Medication Review
Discuss with your healthcare provider if medications or supplements you take may increase bruising. Avoid or reduce NSAID or aspirin use if safe to do so.
Skin Care
Use gentle moisturizers to improve skin elasticity. Avoid harsh soaps or hot water. Limit sun exposure to reduce skin thinning from UV damage.
When to Seek Specialist Care
Refer to hematology if platelet disorders, clotting factor deficiencies, or blood cancers are suspected. Consult dermatology for skin fragility disorders or vasculitis. Rheumatology consultation may be needed if autoimmune systemic disease is identified. Pediatric or social services referral is essential if child abuse is suspected.
Real‑World Examples / Scenarios
Scenario 1
A 45‑year‑old office worker notices recurring small purple bruises on her forearms over several weeks. She denies injury but mentions starting a new herbal supplement containing ginkgo biloba and fish oil. Lab tests are normal. Discontinuing the supplements leads to resolution of bruising.
Scenario 2
An elderly man living alone presents with large, non‑tender bruises on his arms. He takes warfarin for atrial fibrillation and is on a high dose. His INR is elevated. Warfarin dose adjustment brings his INR into therapeutic range, and bruising diminishes.
Scenario 3
A 7‑year‑old child exhibits unexplained bruises on legs and trunk with fatigue and low‑grade fever. CBC shows thrombocytopenia and blasts on the smear. Bone marrow biopsy confirms acute leukemia. Prompt treatment is initiated.
Scenario 4
A middle‑aged woman with easy bruising, gum bleeding, and corkscrew hair is found to have low vitamin C levels. Diagnosis: scurvy. Dietary counseling and vitamin supplementation lead to improvement.
Scenario 5
A teenage athlete with frequent nosebleeds and easy bruising is found to have von Willebrand disease after lab testing. Desmopressin (DDAVP) is prescribed to reduce bleeding episodes, and management plans are adjusted accordingly.
Myths and Misconceptions
Bruising Always Means Abuse
Not necessarily. While bruising can be a sign of child abuse, especially in immobile children or concerning patterns, many unexplained bruises stem from benign or treatable medical causes. Medical evaluation should proceed with sensitivity and evidence.
All Supplements Are Harmless
Herbal or over‑the‑counter supplements may interact with medications or affect clotting. Always inform your provider of all supplements.
If Platelet Count Is Normal, It Can’t Be a Bleeding Disorder
Platelet function disorders or clotting factor deficiencies may still cause bruising even when platelet count is normal.
Supplements Heal Bruises Faster
While vitamin C or arnica may help, they are not miracle cures. Healing depends on the underlying cause and natural tissue repair.
FAQs (Frequently Asked Questions)
How long should a normal bruise take to heal?
Typically, 2 to 3 weeks, gradually changing color and fading. Very large or deep bruises may take longer.
Why do some people bruise more easily than others?
Factors include thinner skin, genetics, medications, nutritional deficiencies, vascular fragility, or underlying medical conditions.
Can stress or emotional factors cause bruises?
Stress alone doesn’t cause bruises, but factitious bruising (self‑inflicted) or psychosomatic factors may play a role in some cases.
Are there any home remedies proven to help bruises?
Cold compresses (first 48 hours) and later warm compresses, topical arnica, and adequate nutrition may offer mild benefits.
Should I worry about a single small bruise?
No—unless it’s accompanied by other troubling signs or lasts unusually long. Most single, minor bruises are harmless.
Summary and Key Takeaways
Unexplained bruises—especially when frequent, large, or associated with other symptoms—can be a sign of underlying medical issues, such as clotting disorders, nutritional deficiencies, systemic disease, or medication effects. A thorough history, physical exam, and targeted laboratory workup help identify the cause. Treatment ranges from simple lifestyle adjustments and supplements to more advanced medical management. Special populations—especially children and the elderly—require careful evaluation and tailored approaches. Prevention through dietary support, medication review, environment modification, and skin care can reduce risk. When in doubt, seek guidance from a healthcare provider.
By understanding the various causes, knowing when to be concerned, and taking appropriate action, you can better manage unexplained bruises and maintain your overall health.